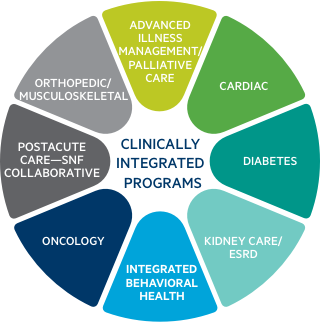
Population-based clinically integrated care models are critical for delivering high-quality value-based care.
In value-based arrangements, coordination and collaboration among providers across the care continuum is a key aspect of being able to enable effective population health management. Montefiore has developed several innovative, population-based clinically integrated care models.
Clinically Integrated Care is at the Core of Effective Primary, Specialty, and Post-Acute Care Delivery
Diabetes
Our Diabetes program supports the practitioner-patient relationship and plan of care. It primarily emphasizes the prevention of exacerbations and complications using cost-effective, evidence-based practice guidelines and patient empowerment strategies. Certified Diabetes Care and Education Specialists are integrated within a multidisciplinary team to provide individualized outreach to identified high risk patients. Our team works closely with the patients to help them attain target clinical outcomes and provide ongoing education, support and monitoring. Key program goals and highlights include the following:
- Provide patient assessment to identify educational needs & generate care plan
- Help patients identify self-management goals & overcome barriers to treatment.
- Screen for key diabetes measures & facilitate annual eye and foot examinations
- Reinforce provider care plan and facilitate patient–physician communication
- Serve as a liaison for patients requiring assistance with medication management, psychosocial and financial issues.
- Assist patients with blood glucose monitoring and assist insulin titration when indicated.
- Provide patients with educational mailings & healthy eating habits
- Facilitate referrals to Community based programs
Oncology Care 360
We offer coordinated oncology care to patients at every stage of their disease. Key program goals and highlights include those listed below:
- A “Call Us First” campaign with a single, toll-free number and use of a dedicated urgent intervention team
- Care management services' Oncology Care Model (OCM) as an important value-based care (VBC) component to encourage practices to work together to address the complex care needs of Medicare patients
- Clinical trials availability and integration
- Consistent clinical pathway deployment
- Multidisciplinary care (medical, radiation and surgical oncology)
- Patient-centered care
- Nutritional counseling
- Psychosocial management
- Screening and prevention
- Supportive/Palliative care
- Survivorship
- Seamless coordination and referrals across sites
Montefiore Integrated Kidney Care and End-Stage Renal Disease (ESRD) Program
Our Kidney Care program and End Stage Renal Disease (ESRD) program emphasize early identification and engagement in order to empower patients and improve health outcomes in our high-risk patients with chronic kidney disease (CKD) and end stage renal disease (ESRD). Key program goals and highlights include:
- Optimizing patient and caregiver knowledge and self-management skills
- Delaying the progression of CKD
- Educating patients and caregivers about CKD prognosis and treatment options and managing the transition from CKD to end stage renal disease (ESRD) with an emphasis on
- Early referral to transplantation
- Timely arteriovenous access placement
- Improvement in home dialysis modality utilization.
- Improved survival
- Reduction in avoidable hospitalizations and emergency room visits
- Improved health-related quality of life
- Improved patient experience with care.
Advanced Illness Management/Palliative Care
The Advanced Illness Management (AIM)/Palliative Care program is enabled by a specialized CMO team that identifies, screens and refers appropriate patients to hospice and palliative care services. Key program goals and highlights include the following:
- Advanced hospice screening and identification of patients using criteria
- Enhanced EPIC EMR capabilities to document and access advance care planning documentation
- Increased hospice liaison presence in acute and outpatient care settings
- Leveraging numerous referral sources, including hospital discharge planners, doctors, the inpatient palliative care team, CMO case managers, postacute discharge calls
- Moving palliative care further upstream
- Realigning resources of palliative care inpatient service to focus on more complex cases
- Robust palliative and hospice education activities, including advanced communication skills for generalists and other providers
Postacute Care—MHS SNF Collaborative
Montefiore Health System (MHS) has formed a special relationship with a number of skilled nursing facilities (SNFs) in the Bronx and in Westchester, Rockland and Orange counties for patients who are leaving the hospital through its MHS SNF collaborative, comprising nearly 40 high-performing SNFs. Key program goals and highlights include the following:
- Commitment to continuous quality improvement
- Effective, high-quality and efficient patient care and transitions
- Integrated operational meetings to share best practices and continuous performance improvement
- Mutual commitment to patient satisfaction and to meeting individual patients' needs
- Optimization of the length of stay across the care continuum
- Reduction in avoidable readmissions
- Structured care transition workflows supported by leading-edge technologies
Integrated Behavioral Health
MHS leverages a comprehensive, highly integrated network of psychiatrists, social workers and care managers to provide accessible and integrated behavioral health solutions. Key program goals and highlights include those listed below:
- An emphasis on patient satisfaction with improved knowledge of self-management
- Crisis management resources, virtual mental-health care and telepsychiatry to help individuals at any time in any location
- Designed for members with both complex medical and behavioral health (BH) needs
- Leveraging advanced technology, such as telehealth, to maximize resources and improve between-visit care
- Same-day appointments and onsite services available, with a large network of over 1,500 behavioral health providers
- Supports BH integration at the primary-care level
- Use of models across a broad range of behavioral health conditions, including depression, general anxiety disorder (GAD), panic, post-traumatic stress disorder (PTSD), social anxiety, alcohol use, attention-deficit/hyperactivity disorder (ADHD)
- Utilization of innovative payment and service delivery models
Orthopedic/Musculoskeletal
Montefiore’s Orthopedic and Musculoskeletal value-based programs are available for elective surgeries and include all procedures listed in the major joint replacement diagnosis group. Montefiore is one of eight Joint Commission-certified orthopedic programs in New York State—and the only one in the Hudson Valley. Key program goals and highlights include these:
- A focus on discharging the majority of patients to their homes with appropriate rehabilitation services, thereby avoiding expensive inpatient rehab stays
- Board-certified orthopedic specialists who focus their practice on hip- and knee-replacement surgery
- Concierge service with dedicated care managers from a patient’s presurgical evaluation through postsurgical rehabilitation and full recovery
- Evidence-based clinical pathways leveraged to perform over 1,800 joint-replacement surgeries each year
- More predictable costs and outcomes
- Reduced days away from work
- Reductions in surgical complications and postsurgery visits or hospitalization
Cardiac
Our Cardiac program integrates CMO care managers with an interdisciplinary team of cardiologists, hospitalists, clinical nurse specialists, dietitians, physical therapists and cardiovascular nurses. This program helps support a team of caregivers who assist patients during and after their hospital stays to ease recovery and reduce the risk of readmission. Key program goals and highlights include the following:
- Pharmacist led care transitions visits spanning inpatient and outpatient setting
- Comprehensive patient education including understanding causes of heart failure, symptom identification, medication adherence, dietary modifications, incorporating exercise and managing stress
- Weight monitoring via patient report or remote patient monitoring
- Smoking cessation counseling and interventions
- Emergency Department navigation resources and supporting resources
- Comprehensive care management and care coordination between care settings
- Advance care planning and ongoing coordination

